Introduction: Understanding Ulcerative Colitis and the Promise of a Plant-Based Diet
This is your guide to a plant-based diet for ulcerative colitis.
Now
I’m so glad you’ve found your way here.
If you have ulcerative colitis or know someone who does, you know the challenges it brings. It’s a journey I understand can be incredibly frustrating and, often, quite isolating.
What if I told you there’s a strong tool in your kitchen that can boost your well-being?
I’m thrilled to dive into the fantastic benefits of a plant-based diet for ulcerative colitis with you today.
What is Ulcerative Colitis, Anyway? My Experience with the UC
Let’s start by getting on the same page about what we’re dealing with.
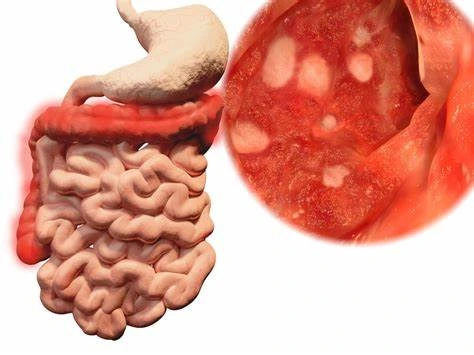
Ulcerative colitis, or UC, is a chronic inflammatory bowel disease (IBD) mainly affecting the large intestine, colon, and rectum. The colon lining becomes inflamed and forms small ulcers.
When I say “inflamed,” I mean it can cause many uncomfortable symptoms. These include persistent diarrhoea, abdominal pain, urgent bowel movements, and sometimes bleeding.
Source: Mayo Clinic
For many, including myself, UC can impact daily life, challenging even simple activities.
Medications are vital for managing symptoms and reaching remission. Still, I’ve always felt I could do more to help my body.
The Emerging Role of Diet in Managing My Ulcerative Colitis Journey
For a long time, diet advice for ulcerative colitis was a mystery. You’d hear vague suggestions but nothing truly concrete. However, there’s been an exciting shift in perspective over the past few years.
More people in the medical field, including those with UC, know that diet is key for managing our condition.
This is where the concept of a “plant-based diet for ulcerative colitis” shines. It’s not only about avoiding trigger foods. It’s also about choosing foods that heal, soothe, and support your gut.
Exploring a plant-based approach can help us manage UC better and boost our quality of life. It’s a journey of discovery, and I’m here to share what I’ve learned along the way.
The Anti-Inflammatory Power of a Plant-Based Diet for Ulcerative Colitis
If you’re like me, you get ulcerative colitis, which is all about inflammation.
So, the next question is, “How do I fight it?”
This is precisely where a plant-based diet truly shines. Shifting my focus to powerful anti-inflammatory foods was a game-changer for me.
I’m explaining here why it’s such a crucial part of managing my UC.
Unpacking Inflammation in Ulcerative Colitis: My Gut’s Battle
First, let’s talk a little more about inflammation itself.
In ulcerative colitis, we’re not just talking about the temporary redness you get from a cut. This is chronic, ongoing inflammation in the colon lining, which can lead to damage over time.
It’s like a fire inside that keeps burning. It leads to all those uncomfortable symptoms I mentioned before. Realising that what I eat could fuel or dampen my energy was a big moment for me.
Certain foods can act like gasoline, while others are like soothing balm. That’s why a plant-based diet is key to my plan for ulcerative colitis.
Key Anti-Inflammatory Components in My Plant-Based Diet for Ulcerative Colitis
Eating anti-inflammatory foods showed me that plants contain compounds that lower inflammation.
Here’s what I’ve found to be particularly beneficial:
Rich in Phytonutrients and Antioxidants: My Plant-Based Allies
What stood out to me about a plant-based diet for ulcerative colitis is its richness in phytonutrients and antioxidants. These are the natural compounds that give fruits and vegetables their vibrant colours.
I love grabbing berries, dark leafy greens, and cooked carrots. They’re full of protective nutrients and work hard in our bodies to neutralise free radicals. These chemicals that aren’t stable can hurt cells and cause inflammation. It’s like having a little army inside me, constantly cleaning up the mess!
Harnessing Omega-3 Fatty Acids: My Plant-Based Inflammatory Boost
When discussing anti-inflammatory fats, our minds often jump straight to fish oil. However, I’ve found excellent plant-based sources of omega-3 fatty acids that also work well to reduce inflammation.
I like to use ground flaxseeds, chia seeds, and hemp seeds. I often sprinkle them on my oatmeal or blend them into smoothies.
These tiny seeds have alpha-linolenic acid (ALA), an omega-3. The body can change ALA into the anti-inflammatory EPA and DHA.
It’s a great way to get essential fats without using animal products. This is a big plus for my plant-based diet with ulcerative colitis.
The Complex Role of Fibre in My Ulcerative Colitis Diet
Fibre is a nuanced topic for us with UC, especially during a flare. In remission and during milder times, I’ve found that fibre from a plant-based diet is vital for gut health in ulcerative colitis.
- Soluble Fibre: This is my friend! Foods like oats, psyllium, and certain cooked fruits (like peeled apples) contain soluble fibre. It dissolves in water to make a gel. This gel helps regulate bowel movements and feeds the good bacteria in my gut. These bacteria produce short-chain fatty acids (SCFAs). SCFAs are vital for gut lining health and have potent anti-inflammatory effects.
- Insoluble Fibre: This fibre comes from the skins of fruits and veggies. When I have a flare-up, it can be tougher for me because it adds bulk to my stool. I usually limit it when I’m sensitive. But when I’m feeling better, I slowly add it back. A healthy gut needs balance. It’s all about listening to my body, a key part of my plant-based diet for my ulcerative colitis journey.
Prebiotics and Probiotics: Nurturing My Gut Microbiome with a Plant-Based Diet
One exciting benefit of a plant-based diet for ulcerative colitis is its support for a healthy gut microbiome.
Plants are full of prebiotics, food for good gut bacteria. When good bacteria thrive, they control harmful bacteria. They also support a strong gut barrier and improve overall gut health. It’s an incredibly symbiotic relationship.
Knowing that every plant-based meal I choose helps create a healthier gut feels great. This knowledge is truly a foundational piece of managing my UC effectively.
Navigating Dietary Choices: Foods to Embrace in a Plant-Based Diet for Ulcerative Colitis
After learning about plants’ anti-inflammatory power, I focused on what to eat.
My journey with a plant-based diet for ulcerative colitis started here. It’s not only about what to avoid. It’s also about celebrating the many nourishing foods that help me feel great.
Let me walk you through some of my favourite and most beneficial choices.
Prioritising Whole, Unprocessed Plant-Based Foods for Ulcerative Colitis Wellness
This is the biggest takeaway for me: simplicity is key.
When I plan meals for my plant-based diet for ulcerative colitis, I always aim for whole, unprocessed ingredients.
This means picking fresh fruits, veggies, legumes, and grains naturally. Avoid packaged foods.
I’ve noticed that processed foods can upset my system. They often contain artificial additives, emulsifiers, and refined sugars. For example, I always avoid carrageenan!
Using fresh, minimally processed ingredients gives my gut the best fuel. This helps me manage my UC.
My Go-To Tolerated Fruits and Vegetables for Ulcerative Colitis
Preparation is key with fruits and vegetables, especially during a flare.
I sometimes struggle with raw veggies. However, I find cooked, peeled, and softer ones easier to digest. And I often eat well-cooked sweet potatoes, silky spinach, and peeled cucumber. I blend the spinach into soups or smoothies.
I love making easy fruit compotes using peeled apples or pears. They are usually well-tolerated. I introduce new items slowly and in small amounts, paying close attention to how my body reacts.
It’s a personal journey.
What works for me might not work for you. Still, these are good starting points for a plant-based diet if you have ulcerative colitis.
Incorporating Legumes and Lentils in My Plant-Based Diet for Ulcerative Colitis
Legumes and lentils are key players in a plant-based diet. They provide great plant protein and soluble fibre.
At first, I was cautious about the fibre content. But I learned that proper preparation helps. I thoroughly soak dried beans and lentils before cooking them until they are very soft. Red lentils are an excellent choice for me. They cook quickly and are easier to digest. I use them to make comforting soups, stews, and even simple lentil purees.
They are crucial and versatile for a nutrient-rich plant-based diet for ulcerative colitis.
Selecting Whole Grains and Pseudograins for Ulcerative Colitis Management
Grains often get a bad name, but some are easy on my stomach and provide important energy and nutrients.
My top choices are white rice and well-cooked oats. White rice is easy to digest. I especially like oats in porridge form.
Quinoa is another fantastic pseudograin that’s complete in protein and often well-tolerated. During flare-ups, I stick to these lower-fiber options.
I may slowly add small amounts of other whole grains when I’m in remission. For example, I tried thoroughly cooking millet. It’s about knowing what my gut can take. I want to enjoy the benefits of wholesome foods in my plant-based diet for ulcerative colitis.
Wise Choices: Nuts and Seeds in My Plant-Based Diet for Ulcerative Colitis
Nuts and seeds are tiny nutritional bombs, and I make sure to include them wisely in my diet. For important anti-inflammatory omega-3s, I use ground flaxseeds, chia seeds, and hemp hearts.
I often add them to my smoothies or sprinkle them over cooked cereals.
I usually choose smooth nut butter over whole nuts, like almond or cashew butter. They are easier to digest, especially during sensitive times.
They offer healthy fats and some protein. Both are key parts of a balanced plant-based diet for ulcerative colitis.
Prioritising Healthy Fats in My Plant-Based Diet for Ulcerative Colitis
Healthy fats are vital for health and can help calm inflammation. My staples include extra virgin olive oil, which I use for cooking and dressing, and avocado oil.
I love avocados. They’re creamy, satisfying, and full of healthy monounsaturated fats. I limit omega-6 vegetable oils, like soybean and corn oil, because I’ve read that they can cause inflammation.
I focus on high-quality, plant-based fats in my diet. They help fuel my gut and support my ulcerative colitis.
Foods to Approach with Caution or Avoid in a Plant-Based Diet for Ulcerative Colitis
I’ve shared my favourite healthy foods from my plant-based diet for ulcerative colitis.
Let’s discuss the other side: the foods I approach carefully or avoid altogether.
This part of my journey is just as crucial for managing my symptoms and staying in remission. Believe me, through trial and error, I’ve learned what my gut doesn’t appreciate!
Identifying My Personal Trigger Foods for Ulcerative Colitis on a Plant-Based Journey
The key lesson I learned about a plant-based diet for ulcerative colitis is simple. What works for one person might upset another.
There’s no one-size-fits-all list of “bad” foods, which can be a bit frustrating initially. Finding my trigger foods has been a journey. It takes careful observation and some detective work.
I highly recommend keeping a food diary when you’re starting. Note down what you eat and how you feel afterwards. Over time, you may see patterns.
Some people handle healthy plant foods well, but raw broccoli makes me uncomfortable. A personalised approach is key to improving your plant-based diet for ulcerative colitis. It’s about listening intently to your body’s unique signals.
Navigating High-Fibre Raw Vegetables and Fruits During Ulcerative Colitis Flares
I love fruits and vegetables, but I’ve learned they aren’t always good during a flare.
High-fibre raw veggies, especially those with tough skins or crunchy textures, can be tough on my inflamed colon. Examples include raw kale, bell peppers, and apple skins. They can increase irritation, gas, and discomfort during these sensitive times.
My strategy is to be very cautious with these when my UC is active. As mentioned earlier, I stick to cooked, peeled, and softer options.
Once I’m in remission and feeling stable, I may slowly add small amounts of raw foods back in. I’ll always check for tolerance.
Balancing fibre in a plant-based diet for ulcerative colitis is tricky. Patience is key.
Why I Steer Clear of Refined Sugars and Sweetened Beverages for Ulcerative Colitis
It might seem obvious, but I avoid refined sugars and sweetened drinks. I’ve noticed that when I consume sugary foods, my gut feels… angry.
Research shows that refined sugar can cause inflammation. It also harms the gut microbiome’s balance.
An imbalanced gut can lead to inflammation. This is precisely what we want to reduce with a plant-based diet for ulcerative colitis.
I must say no to sodas, candies, pastries, and many “healthy” sweetened plant-based yoghurts. If I need a sweet touch, I find that natural sweetness from fruits or a tiny bit of maple syrup or dates works best.
Other Common Irritants I Consider Avoiding for My Ulcerative Colitis
Besides sugar, I now handle these common irritants with care or avoid them in my plant-based diet for ulcerative colitis:
- Spicy Foods: I enjoy a good kick, but very spicy dishes can irritate a sensitive gut. I generally opt for milder flavours to keep my colon happy.
- Excessive Caffeine: Some people are okay with a morning coffee. But for me, too much caffeine can speed up bowel movements and increase urgency. I’ve found herbal teas to be a much gentler alternative.
- Alcohol: This is a big one. Alcohol can directly irritate the gut lining and disrupt the microbiome. For me, avoiding alcohol altogether has been a clear benefit in managing my UC.
Addressing Emulsifiers and Food Additives for My Ulcerative Colitis Management
This is a key point, especially if adopting a plant-based diet for ulcerative colitis.
Many processed foods, including those labelled “vegan” or “plant-based,” have emulsifiers. These can include polysorbate 80 or carrageenan, along with other artificial additives. New studies show these can harm the gut barrier and may lead to inflammation.
This is a significant reason why I prioritise whole, unprocessed plant foods.
I read ingredient labels closely. I watch for hidden additives that might cause problems.
It’s an extra step, but I find it worth it. Knowing I’m doing all I can to protect my gut lining helps me in my journey with ulcerative colitis.
Implementing a Plant-Based Diet for Ulcerative Colitis: Practical Strategies
You’re sure that a plant-based diet helps with ulcerative colitis. You know which foods to enjoy and which ones to be careful with.
That’s fantastic!
But how do you do it?
Switching to this way of eating requires some practical strategies. It’s not about perfection but about consistent, gentle progress.
Let me share some of the approaches that have helped me tremendously.
Starting Slowly and Gradually Transitioning to a Plant-Based Diet for Ulcerative Colitis
It felt overwhelming when I first considered changing my diet for my UC. I quickly learned that the key is to start slowly. Don’t feel pressured to overhaul your entire diet overnight.
For me, it began with small, manageable steps. I might have started by choosing one day a week for plant-based meals. Or, I could have replaced my usual breakfast with oatmeal topped with fruits and seeds.
This gradual change helped my digestive system adjust smoothly. This is key for those with ulcerative colitis.
It also let me try new recipes and discover plant-based options I liked.
Could you consider it a marathon, not a sprint? This is key to building a lasting plant-based diet for ulcerative colitis. Listen to your body every step of the way—it will tell you if you’re moving too fast.
My Approach to Meal Planning and Preparation for a Plant-Based Diet for Ulcerative Colitis
Once I embraced this lifestyle, I found that meal planning and prep became my best friends.
It may seem harsh, but it makes things easier. I always have safe, healthy choices on hand.
I often dedicate a couple of hours on a Sunday to:
- Batch cooking: I’ll make a big pot of quinoa or brown rice, roast sweet potatoes or butternut squash, and prepare my favourite lentil soup. This way, I have ready-to-eat components for quick meals throughout the week.
- Simple Recipes: I focus on recipes with fewer ingredients that are easy to digest. Think simple vegetable purees, steamed greens, or easily digestible fruit smoothies.
- Ingredient Sourcing: I keep my pantry stocked with staples, including dried lentils, oats, quality olive oil, and my favourite plant-based milk.
This proactive plan helps me stay on my plant-based diet for ulcerative colitis, even on busy days. It stops me from grabbing less healthy options just for convenience.
It also helps me get a variety of nutrients. I focus on B12, iron, calcium, and Vitamin D, which require more planning when following a plant-based diet.
Hydration and Supplementation Considerations for My Ulcerative Colitis Journey
I’ve realised that staying hydrated is crucial for my gut health, especially with UC.
I try to drink a lot of water every day. Herbal teas like ginger or peppermint can also help me relax and get more fluids. I stress the need for professional advice for supplements.
A good plant-based diet can be rich in nutrients for ulcerative colitis. I talk about specific supplements with my healthcare team.
For example, people on a plant-based diet often need a B12 supplement. My doctor and I also monitor my Vitamin D and iron levels, which can be of concern to UC patients. Omega-3 supplements derived from algae are another common consideration for anti-inflammatory support.
If you have IBD, you should always consult your doctor or a certified dietitian before taking any new supplements.
Why I Work Closely with Healthcare Professionals for My Plant-Based Diet for Ulcerative Colitis
Finally, I want to emphasise how important it is to work with my healthcare team.
I love my plant-based diet for ulcerative colitis, but I always follow medical advice, too.
My gastroenterologist manages my UC treatment. They check my inflammation markers and explain when I may need to adjust my medication. Crucially, I also work with a registered dietitian who specialises in IBD.
They’ve been invaluable in helping me:
- I want to personalise my diet further, considering my unique triggers and nutritional needs.
- Ensure I’m getting adequate nutrients and preventing deficiencies.
- Navigate challenges and make adjustments during flares or periods of remission.
This team approach gives me the best care. It mixes dietary changes with regular medicine, and it’s genuinely the most effective way I’ve found to manage my ulcerative colitis and thrive.
Beyond Diet: Holistic Management of Ulcerative Colitis
Focusing on a plant-based diet has dramatically helped my ulcerative colitis. However, I realise it’s just one piece of the bigger puzzle.
My UC journey has taught me that true well-being comes from nurturing my whole self. For me, that means going beyond my diet. I also focus on other essential parts of holistic health. Let me share what else I’ve found incredibly helpful in managing my condition.
Prioritising Stress Management for My Ulcerative Colitis Wellness
This is a big one for me and, frankly, for many people living with IBD. I’ve personally experienced how stress can directly impact my gut.
It’s well-known that our brains and guts are closely linked. This link is often called the gut-brain axis. When I’m stressed, my UC symptoms usually get worse, even if I stick to my plant-based diet for ulcerative colitis.
So, I must add stress management techniques to my daily routine. Meditation for 10-15 minutes daily calms my nervous system.
Yoga is another fantastic tool for me. It helps to release tension and improve my sense of calm. Even simple deep breathing exercises throughout the day can make a difference.
Focus on what helps you relax. Make it a regular habit to manage your ulcerative colitis better.
The Underrated Importance of Adequate Sleep for My Ulcerative Colitis
Sleep may seem passive, but it helps my body heal and manage inflammation. When I don’t get enough quality sleep, I feel it in my entire system; my gut is no exception.
People with ulcerative colitis should be worried since not getting enough sleep might hurt their immune system and worsen inflammation.
I prioritise getting 7-9 hours of restful sleep each night. This means establishing a consistent sleep schedule, making my bedroom a comfortable, dark, and quiet sanctuary, and winding down before bed (no screens!).
It’s incredible how much more resilient I feel, both physically and mentally, when I’m well-rested. Good sleep is a powerful ally in my holistic management of ulcerative colitis.
Embracing a Supportive Environment for Ulcerative Colitis Management
It’s hard to live with a long-term illness like ulcerative colitis. A strong support system can make a big difference.
Dealing with symptoms and dietary restrictions can make you feel alone. The unpredictable nature of UC adds to this feeling.
Connecting with family and friends who understand (or at least try to understand!) what I’m going through has been invaluable.
I’ve found support and advice in online and in-person groups, not just from friends.
Sharing experiences with people who understand can lessen loneliness and offer fresh views.
It’s empowering to know you’re not alone on this journey.
Supportive people and resources are key to managing my ulcerative colitis. This approach works well with my plant-based diet and other self-care practices.
Frequently Asked Questions about a Plant-Based Diet for Ulcerative Colitis
On my journey with ulcerative colitis and a plant-based lifestyle, many have asked me about this choice.
It’s normal to have doubts and want clarity, especially when managing a complex condition like UC with diet changes.
Let’s tackle some common questions about a plant-based diet for ulcerative colitis.
A. Is a Plant-Based Diet for Ulcerative Colitis Suitable for Everyone?
This is one of the first questions I usually get, and it’s important. From my experience, a plant-based diet for ulcerative colitis can be amazing. It worked wonders for me. But it’s not a one-size-fits-all solution. It may not fit everyone the same way. Each person’s body and ulcerative colitis are unique. What one person tolerates beautifully, another might find challenging.
For example, I like some cooked vegetables, but others may struggle with them during a flare-up. It’s crucial to remember that this is a highly individualised journey.
Always discuss significant dietary changes with your gastroenterologist. It’s also best to include a registered dietitian who knows about IBD. They can help determine if this approach suits you and guide you safely.
B. Can a Plant-Based Diet for Ulcerative Colitis “Cure” My Condition?
Oh, I wish there were a “cure” for ulcerative colitis! I’ve asked myself this question many times.
In my experience, a plant-based diet helps manage ulcerative colitis effectively, but it is not a cure. Ulcerative colitis is a chronic, long-lasting condition.
I’ve found that a plant-based diet helps me reduce symptoms, extend remission, and boost my quality of life. It helps me control my gut’s inflammation and support a healthier microbiome.
It hasn’t cured me, but it has changed how I live with UC. Now, it’s more manageable, and I can thrive more often. It’s about empowerment and control, not necessarily eradication.
C. How Quickly Will I See Results on a Plant-Based Diet for Ulcerative Colitis?
This is another common inquiry, and I understand the desire for quick relief! When I started my plant-based diet for ulcerative colitis journey, I was eager to see changes. The reality is there’s no fixed timeline. Some people may notice slight changes in just a few weeks. For others, it might take several months to feel significant differences.
My advice?
Be patient and consistent. It’s not usually an overnight fix. Your gut needs time to heal, inflammation takes time to go down, and your microbiome needs time to rebalance.
Focus on the long game and celebrate small victories along the way. Even minor reductions in symptoms or improvements in energy can be huge wins.
Believe in the process. Remember, slow and steady change is usually the best way to go.
D. What if I Can’t Tolerate Certain Plant-Based Foods on My Plant-Based Diet for Ulcerative Colitis?
This is a very valid concern, and I’ve personally navigated it. It’s normal for some plant-based foods to upset your stomach, especially with UC.
As I mentioned before, it’s about individual tolerance. If plant food makes you uncomfortable or bloated or worsens your symptoms, avoid it.
The beauty of a plant-based diet for ulcerative colitis is its incredible variety. There are so many options! If raw kale is a no-go, try cooked spinach. If lentils cause issues, maybe focus on well-cooked white rice or oats.
Don’t feel discouraged if you have to eliminate a few healthy plant foods. The goal is to find plant-based foods that work for your unique body and build your diet around those. Feel free to try new things. Also, talk to your dietitian for advice that fits you.
E. Do I Need to Take Supplements on a Plant-Based Diet for Ulcerative Colitis? My Supplement Strategy
The answer is usually yes, but there is a big asterisk: always with professional help.
A well-planned plant-based diet for ulcerative colitis is nutritious. However, some nutrients can be tough to get from plants alone. Also, UC may impact how well your body absorbs them.
Based on my talks with my doctor and dietitian, I take a Vitamin B12 supplement because it mostly comes from animal products. I also check my Vitamin D levels regularly and take supplements if needed. This is common for many people, no matter their diet. It’s especially true here in South Africa, where sun exposure can change.
Sometimes, my doctor suggests iron or an omega-3 supplement from algae based on my blood tests.
My golden rule is to get my levels checked by my healthcare provider before adding new supplements to my routine.
It’s about smart supplementation that supports my diet. It helps me meet my nutritional needs for managing UC.
Conclusion
I hope you feel informed and empowered. Dietary changes, especially a plant-based diet, can help manage ulcerative colitis.
My journey has taught me that UC is tough. Yet, we have strong tools to help us. These tools go beyond medication and include how we nourish our bodies daily.
Recapping the Benefits of My Plant-Based Diet for Ulcerative Colitis Journey
Looking back, choosing a plant-based diet for ulcerative colitis has dramatically impacted my health.
I’ve felt the enormous benefits myself: less inflammation, a happier gut, and a boost in my overall well-being that I never expected. Focusing on whole, unprocessed plant foods can calm the internal storm of UC. It’s incredible how effective this can be.
This dietary change has led to fewer painful flares, more predictable days, and better control over my condition. It’s a journey of discovery. It takes effort and attention, but the rewards for my gut health and quality of life are immense.
Emphasising Individualised Approaches and Professional Guidance for Ulcerative Colitis
But remember, each body is unique, and our experiences with ulcerative colitis are, too. A plant-based diet for ulcerative colitis isn’t one-size-fits-all.
What works well for me may need some tweaks for you, and that’s fine.
I can’t stress enough how important it is to work with your healthcare team.
Your gastroenterologist and a knowledgeable dietitian who understands IBD are your best allies.
They can help you tailor this approach and will monitor your progress and make sure you meet your nutritional needs.
The team will also safely integrate dietary changes with your medical treatment plan. Their guidance is essential for optimising your ulcerative colitis wellness journey.
A Message of Hope and Empowerment for Those with Ulcerative Colitis
I want to share a message of hope and strength with everyone with ulcerative colitis.
Managing UC can be tough, but taking charge can help. Try a plant-based diet for ulcerative colitis. This choice can boost your sense of control and lead to a healthier, more vibrant life.
It’s a journey, not just a destination. It’s all about learning, adapting, and listening to your body. Make smart choices. Eat healthy foods. Manage stress. Get enough sleep. Build a support network. These steps boost your wellness with ulcerative colitis.
You are not alone; many avenues exist to help you feel better and thrive.
I invite you to start this journey with an open mind. Also, commit to caring for your amazing body.